COVID-19 Outlook: Stepping Up Safety During a Period of Uncertainty
Here are the main findings from this week’s update to our COVID-Lab forecasting model:
- The nationwide average PCR testing positivity rate was 5.2% this past week, unchanged from the week prior. Nearly half of the 819 counties in our model had a higher testing positivity rate this week than last week, concentrated mostly in the Upper Midwest, Northeast and Mid-Atlantic.
- The country’s average county-level reproduction number (a measure of transmission that indicates how many additional individuals could be infected by every positive case) is hovering at 1, up from 0.93 last week. Nearly 40% of the counties included in our model now have a reproduction number of 1, again concentrated mostly in the Upper Midwest, Northeast and Mid-Atlantic.
- The number of counties below a weekly incidence of 100 cases per 100,000 individuals dropped to 43% this past week; however, we also saw a 5% increase in the number of counties included in our model that have fewer than 50 weekly cases per 100,000 individuals.
- Nearly 40,000 COVID-19 patients remain hospitalized in the country, mostly unchanged from last week, and adult admissions have stalled at over 10,000 daily. New pediatric admissions have plateaued after several weeks of decline.
Specific areas of concern:
- Emergency department visits and hospitalizations are increasing in Michigan. Wayne (Detroit), Genesee (Flint), and Macomb counties have reproduction numbers over 1.3, indicating substantial transmission. Our models project a potential doubling in case incidence in these counties during the next 3-4 weeks.

Above are the projections for Macomb County in Michigan.
- Both case incidence and testing positivity are increasing again in many midwestern cities, including Minneapolis and Chicago, although absolute case incidence and rate of growth are below large urban counties in Michigan.
- Testing positivity and case incidence are increasing in metropolitan areas along the I-95 corridor. Transmission is increasing in the Washington, D.C. metro area, accompanied by modest increases in emergency department visits and hospitalizations over the last couple of weeks. New York City and surrounding communities continue to see sustained high case incidence and reproduction numbers that are hovering just above 1, with modestly increasing test positivity. In Boston, reproduction numbers are still just below 1 and case incidence has remained flat over the last couple of weeks.
- After many weeks of declining numbers, test positivity is increasing again in Phoenix, San Diego, Los Angeles and Las Vegas. Our models foresee persistent case incidence rates in this region over the next four weeks, and growing case incidence in Las Vegas.
- While many Florida counties continue to see declining test positivity, reproduction numbers are increasing again slowly in some areas. Our projections for coastal regions, including Miami and Tampa Bay, forecast modest increases in case incidence in the coming weeks.
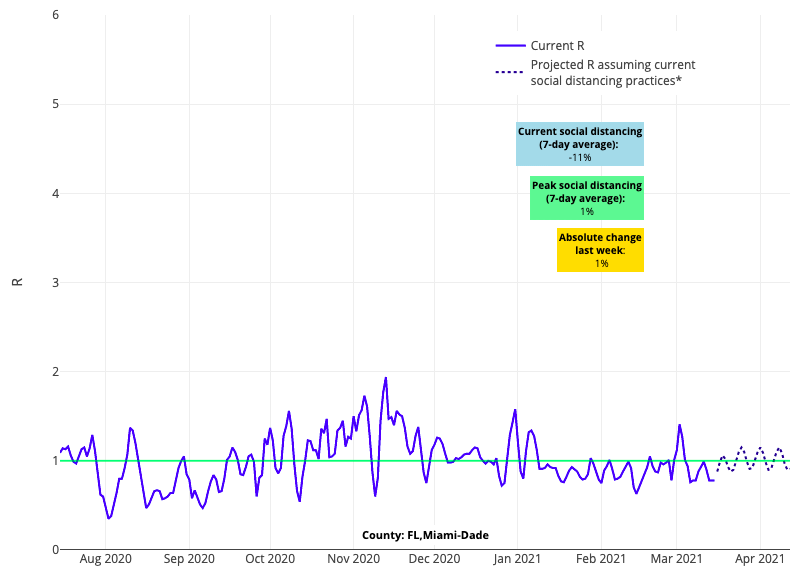
Above is the reproduction number projections graph for Miami-Dade County in Florida.
- Our models are detecting a risk for increasing case transmission in Hawaii in the coming weeks, although overall incidence remains lower than other areas of the country.
The First Signs of a Potential Spring Resurgence Should Not Deter School Reopening
Looking at the data this week, we can see that our country remains very much in a period of sustained COVID-19 transmission. Although increases in transmission are somewhat expected as communities begin to reopen, these trends are concerning and a reminder that this pandemic is far from over. We will need to monitor the duration and amplitude of this evolving resurgence in the coming weeks. As we have been warning, too rapid of a return to normal (e.g., removing mask restrictions and allowing for larger gatherings) will most certainly result in continued increases in case incidence.
The regions of most concern right now are metropolitan areas. This is likely because they are more densely populated, facilitating easier viral transmission and making it more difficult to achieve higher population-level vaccination rates. However, these concerning data trends coupled with circulating variant strains should prompt efforts to increase vaccine inventory and distribution to these more crowded communities.
The stalled improvements in test positivity and case incidence across the country come at a time when many schools are resuming in-school instruction for more students. This will lead to questions about whether continuing to reopen schools is appropriate. For multiple reasons, we are still confident that moving to in-school instruction as much as possible is the right thing to do:
- First, the increases in transmission that our models predict in the coming weeks are not of the same intensity as we saw this winter.
- Second, focused vaccination efforts are allowing many school staff to be vaccinated.
- Finally, there are accumulating reports (with more data to be released soon) that demonstrate very low risk for secondary infections (sometimes referred to as the secondary attack rate) among students, particularly younger ones, who are exposed at school while wearing masks appropriately, even at distances under six feet. These data tell us that linked in-school transmission can be prevented with strong safety protocols. So long as schools and health departments are carefully contact tracing school-based exposures, they will have the necessary data to confirm whether this remains true.
Teachers are now being vaccinated: What does that mean for school safety plans?
Our team is receiving questions about how the increasing vaccination of school staff might influence schools’ plans for spring. Certainly, the vaccination of school staff has helped accelerate plans for returning to full in-school instruction. However, we are advising schools that vaccination of school staff should not obviate continued commitment to other layers of their safety plan; staff vaccination will not eliminate the risk posed when classrooms become more fully populated. At this time, the risk of complacency with respect to mitigation plans may be the biggest threat to successfully expanding in-person instruction, particularly in upper grades where behavior and susceptibility could conspire and lead to linked in-school transmission.
As more children enter the school building, it is inevitable that the distance between students at any given time will decrease. We would emphasize that if we intentionally allow one mitigation strategy to weaken—in this case distancing—schools must strengthen or reinforce other layers of the safety plan to retain a similar level of safety. This is particularly important for enforcing the appropriate use of masks among students and staff, reinforcing symptom screening protocols and emphasizing hygiene throughout the day. Finally, even as distancing is reduced to return more children to the building, schools should continue to leverage outdoor or flex space (particularly for lunchtime) to spread children across as much space as possible.
With increasing vaccination of school staff, we have also received questions about whether staff reassurance testing should continue in light of new Centers for Disease Control and Prevention (CDC) guidelines that allow for limited gatherings of vaccinated individuals and an exception for quarantine of exposed individuals who remain asymptomatic after vaccination. These new guidelines for fully vaccinated people only allow for small gatherings in private residences, where the risk of transmission is modest. They differentiate congregate settings, like schools, where assurance testing programs are attempting to halt risk of wider outbreaks by early recognition of infected individuals.
While evidence suggests that the risk of severe disease is almost eliminated, at least in the short run, for vaccinated individuals, the evidence on transmission is more mixed. Experience from other vaccine-preventable diseases suggests that immunization lowers, but may not eliminate, the risk of transmission from vaccinated to unvaccinated individuals. In clinical trials, the Johnson & Johnson vaccine, for example, was terrific at protecting against severe disease, but there remains a 1-in-4 risk of milder infection among the vaccinated. We have also learned from other communicable diseases, like measles, that when the proportion of unvaccinated individuals increases in a region, the risk of transmission to individuals, both vaccinated and unvaccinated, increases.
For that reason, schools would be wise to see the benefit that strengthening testing programs can have during a period of transition to full in-school instruction. This week, Caroline LaRochelle on our policy team (you may remember her terrific review on enforcement challenges for masking mandates last fall) led the authorship of a nuanced review on how schools across the country are incorporating testing into their school safety plans. In our own region, Project: ACE-IT has conducted more than 40,000 tests since January, and that number is quickly growing with the School District of Philadelphia returning last week. Finding only 100 of those tests to be positive reassured all of us that rates of asymptomatic infection are very low in the school settings, but also that this risk persists.
As schools repopulate, assurance testing programs will continue to prioritize adults in the building, vaccines notwithstanding. Community transmission rates persist among working-age adults, and a study published in Pediatrics this past week revealed that 80% of all in-school linked transmission cases in New York City from the late fall involved a contagious adult who acquired infection away from school. However, this emphasis on adult assurance testing, also supported by CDC reopening guidelines, does not preclude schools from providing more testing resources for students—in our region, we focus on athletes, performing artists, and high-risk special education students for whom masking or distancing is difficult. Caroline’s blog post also provides other strategies—from random point prevalence testing of student samples each week to pooled testing strategies that touch all students in the building or among athletic teams. Each has its benefits and tradeoffs, but weekly assurance testing for the highest-risk individuals is the essence of a strong testing program.
The rebound in transmission we are seeing this week is a reminder that the pandemic is not over, and that our resolve and patience to see through this period will be tested. Attention to detail in safety plans is more important now than ever, but the months of experience with safety protocols that schools have accumulated to date have revealed these plans to be effective in providing safe learning environments for children. The data on school safety remains on school leaders’ side, so long as they are prepared to meet the challenge.
