COVID-19 Outlook: Rapid Spread with New Restrictions on the Horizon
As we move past election week, regardless of the conclusion, we urgently need action plans to address accelerating infection rates and compromised contact tracing that may soon irreversibly make our country vulnerable to a long, dark winter.
Our updated models this week confirm that colder weather, particularly in the northern half of the United States, is not simply increasing viral transmission, but also leading to greater severity of disease, much like we saw in March. All states—except Hawaii—have rising hospitalization rates and intensive care admissions, at least half have exponential community spread of COVID-19, and among those, at least six have rapidly accelerating ICU admissions and growing ventilator use. We are also seeing field hospitals emerging in places like El Paso, Texas, and at the Wisconsin State Fair Park. Substantial spread is now threatening our capacity to care for the sick, with or without COVID-19.
Chicago and major cities in Wisconsin, Minnesota, and Michigan are the quickest growing hotspots in the country. Indianapolis and the major cities in Ohio are not far behind their neighbors to the north and west. In western Pennsylvania, demand for ventilators is growing as ICU admissions quickly rise; we suspect that Philadelphia may be just weeks behind. In the Northeast, Connecticut and Rhode Island are already moving toward rapid growth in early November. Finally, in New York, there is clear acceleration of spread upstate—rate of growth in areas like Rochester is eclipsing that of the New York City metro area (although Staten Island is showing signs of resurgence risk).
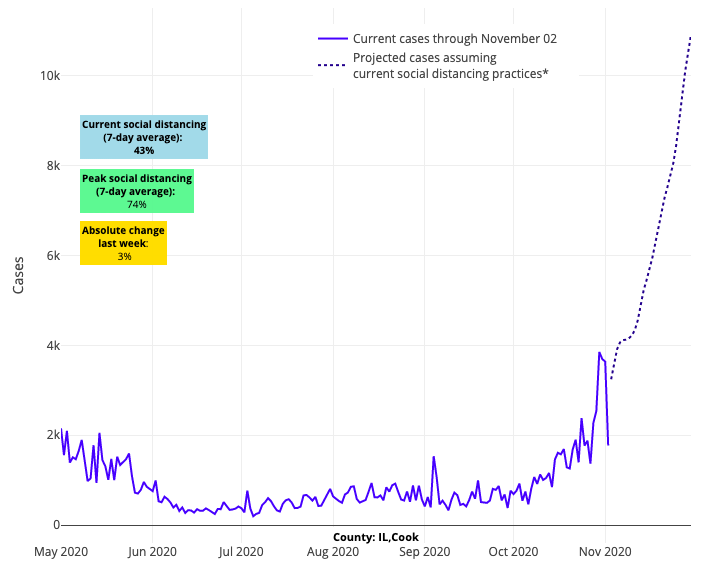
Above are the projections for Cook County (Chicago) in Illinois.
Our models also project growth in viral transmission across southern states, but the forecasts clearly differ from the North in their rate of growth. This suggests that the relative warmer weather in these areas has slowed the pace of transmission and severity of disease from southern New Jersey down to Florida. It's as if the areas of the Mid-Atlantic and South are still in patterns of summer, when hospitalizations were less frequent and shorter, even as caseloads increased. The transition zone between North and South appears to be in the middle of Pennsylvania in the East, and in the hills of the Sierra Nevada and Rocky Mountains in the West.

Above are the projections for Washington D.C.
What makes these observations so frustrating to our team is that these patterns have been emerging for weeks now, met with diminishing intervention from state or city leaders who have been reticent to mount a more robust response to the crisis at their doorstep. It is noteworthy, that some locations did make attempts to reduce transmission through new targeted restrictions, but it appears these interventions were too late.
For example, Chicago recently closed its restaurants to indoor dining and limited gathering sizes to six or fewer people. But this week, their growth in case incidence, hospitalizations, ICU admissions, and ventilator use has grown so dramatically, that it is becoming more likely that a full shelter in place may be necessary to avoid a federal emergency of health care access. Denver, and the state of Colorado at large, reduced its gathering size limit to 10 and moved to limit occupancy of its stores and restaurants to similar levels as the spring. But the infection rates in Denver are not slowing in response, and their hospitalization rate grows unabated.
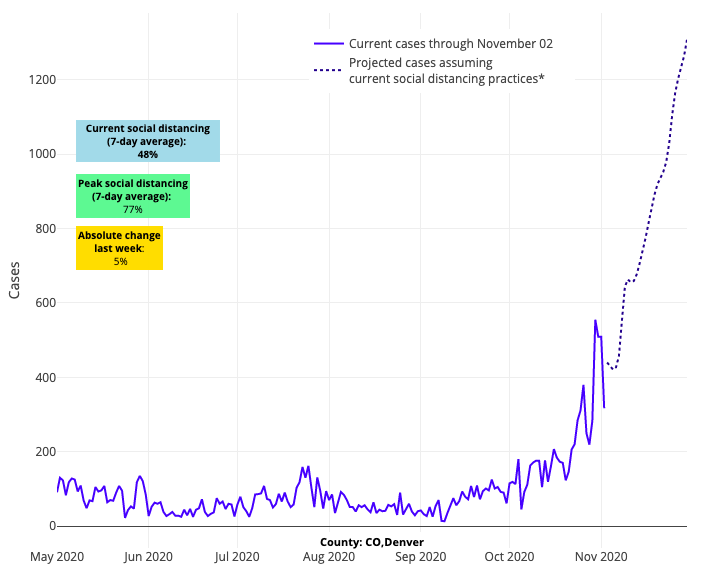
Above are the projections for Denver County in Colorado.
All of this makes for increasing certainty about the dire situation facing the country as we head into winter. It’s time for our state and local leaders to act with targeted mitigation and enforcement strategies. These strategies need to include clear plans for transitioning between in-person schooling and virtual learning during the heights of this wave.
Targeted mitigation and enforcement strategies
As governors and local officials plot their next moves, we know that one of their biggest challenges has been how well they have tethered restrictions to credible enforcement. If restrictions are in place but lack an enforcement strategy, we can expect that the mandates will be ignored. In anticipation of new mandated restrictions with this fall wave, Caroline La Rochelle, a member of our policy team, assessed how cities and states have handled issues of enforcement thus far. Her summation of adherence (or lack thereof) to masking orders and limits on gathering sizes and restaurant/bar occupancy highlights just how difficult it has been to align enforcement activities with the mandates that political leaders have issued.
While this is discouraging, Caroline gives us some hope by hinting at a path forward through the use of targeted enforcement of high-risk activities. We know now that limited restaurant or gym occupancy, or even the operation of hair salons, are not driving this current resurgence. Rather, we are increasingly observing this fall that transmission is happening in small gatherings related to youth sports or among family and friends in their homes. As the weather becomes colder, these gatherings are taking place indoors, often in the absence of strict mask use, creating the perfect conditions for a virus that can spread among people who are crowded into a poorly ventilated space. These events are a sign that pandemic fatigue has set in, beset with mixed messages from political leaders on the value of masking and distancing to contain the resurgence this winter.
Observations from contact tracing efforts provide us important information to combat further widespread transmission. If we choose to leverage this knowledge, we can reduce COVID-19 spread using targeted measures that limit gathering sizes while subverting an immediate need for lockdowns. This includes targeted restrictions on bars (curfews and/or very limited occupancy) and sacrificing large holiday parties this winter. And it’s up to our leaders to enforce these measures—penalizing/citing those individuals and businesses who choose to egregiously ignore the restrictions.
The importance of limiting gathering size is also relevant to youth extracurricular activities, including indoor sports, which we know are causing transmission that spills into the community. In contrast to fall outdoor sports, through which on-field transmission appears to have been limited, we remain uncertain of transmission risk during gameplay indoors, particularly given recent youth hockey outbreaks. The degree of risk for spread on the ice or court is not well defined, but risk of spread on the ice or court exists and likely varies with both the game being played and the level of play. What is certain is that close contact between individuals off the field in locker rooms, buses and carpools, in the stands, and in parking lots has led—and will continue to lead—to transmission events. We will release revised guidelines that consider indoor sports on our website this week.
If youth sports leagues want to preserve any opportunity to keep playing, they need enact mandates that strictly curtail all off-field interaction. However, even with these restrictions, and the potential for on-field spread may be too overwhelming to continue safely with team competition during periods of widespread community transmission, and may need to be sacrificed to preserve in-school learning options, at least until early spring or transmission rates decrease substantially. Already, we saw the state of Massachusetts close their hockey rinks this past week due to an abundance of evidence that youth hockey leagues were serving as a source of community transmission.
We all want to preserve any activity possible for our children during this pandemic, but the lack of communities collectively committing to mitigation strategies has put us in this dire situation.
Upper Limits for Safe Operations of Schools
Last week, we documented the tremendous success that many schools have had with their thoughtful reopening plans. This week, we are armed with new, sobering data that remind us that there is an upper threshold to safe school operations.
As county-level targeted mitigation strategies break down and case incidence and testing positivity rapidly rise, anxiety is mounting among teachers, staff and student families. Our failed commitment to mitigation efforts has undermined the capacity of robust contact tracing programs to ensure that all exposed persons are informed of their risk and counseled to quarantine. This has raised the risk that, even with strong safety protocols, more students, teachers, and staff are unwittingly going to school while incubating or shedding the virus, thus setting the stage for linked in-school transmission.
As case counts and test positivity have increased in many regions, local health officials and superintendents are weighing when to revert to temporary virtual learning. Ideally, school closures would be a last resort given that, at least to date, the empirical data on the degree to which schools are contributing meaningfully to ongoing community transmission in high incidence areas has been incomplete. However, the success of a school community will ultimately be determined by the success of the community at-large. The goal of a transition to virtual learning is safety of the teachers, students and families, while the larger community buckles down with the appropriate mitigation strategies to regain control of viral transmission.
The vigorous debate playing out among school boards right now is how to choose the right moment to revert to virtual learning. In an effort to better understand the complexity of this decision, we met with school districts throughout southeastern Pennsylvania to discuss how to traverse this period of accelerating viral transmission and to clarify parameters that would inform a decision to go to virtual learning. We counseled that first and foremost, each school needs to monitor their county’s case incidence and test positivity rate. If possible, schools should compare these county-wide rates to the rates from the specific communities that are served by the school; if the school’s community rates are markedly lower than that of the county, a school might opt to cautiously continue in-person learning while closely tracking their local data.
However, we are finding this week that in our own metropolitan area of Philadelphia we are seeing regional rates exceed 7% and moving toward the 9% threshold. This is the threshold that our team previously suggested represents widespread and uncontrolled community transmission. As we reach the 9% metric, we are seeing increasing burden of students and teachers with COVID-19 infections with linked transmission events in classrooms. These changes in the past week are validating our recommendations for schools to consider transitioning back to virtual learning to let the height of this wave pass.
In the Philadelphia region, schools and school districts should be proactively planning for a transition to period of distance learning now. There may be several permutations of a virtual learning plan to consider, from full virtual instruction to retaining select populations for in-school learning. Our blog post from last week reviews the many options that are available as schools make this decision, and our guidance for in-school operations includes a list of questions to guide decision-making around this. But, most of all, we would emphasize that teachers and school staff are essential workers and they—and the families that rely on school as a foundational community resource—deserve a consistent approach and transparency to how these decisions will be made.
Until now, we have tried to forestall reverting on our in-school guidance, but with rising transmission and test positivity rates in counties across the country, we fear that local school outbreaks are now increasing in advance of Thanksgiving. While we offer a number of options above for reverting to distance learning, a plan we cannot justify is one that continues full in-school activities until a large outbreak happens. We can only hope that as the election news settles, people realize what is really happening with resurgent caseloads and hospitalizations and commit to proactive targeted mitigation strategies. We are rapidly running out of time if our hope is to protect our communities and extend safe in-school instruction over the winter.
