COVID-19 Outlook: Moving Past Peak During a Period of Fragile Equilibrium
Here are the overall findings from our analysis of the weekly COVID-Lab forecasting modeling data:
- Although down slightly this week, average testing positivity rates across the 821 counties we follow in our model remains high at 13.6%, and half of these counties are still seeing more than 400 cases per 100,000 individuals weekly.
- The top ten states with continued growth in testing positivity rates this past week include Tennessee—which led the way with an increase of 3% to reach nearly 20% testing positivity across its counties—Alabama, Arkansas, Arizona, Georgia, Louisiana, New York, Massachusetts, Oklahoma and Pennsylvania.
- As many areas begin to move past peak, we continue to see elevated risk for the New York City area, where we are forecasting cases could still double in Queens and Kings (Brooklyn) Counties, as well as neighboring Suffolk and Nassau Counties.
- The Southeast also remains a concern, particularly in the Atlanta region (Fulton and Dekalb Counties) where weekly case incidence remains below 300 cases per 100,000 individuals, but their testing positivity rate is increasing—leading to concerning forecasts for resurgence in advance of and immediately following the Christmas holiday.
- While the rate of growth is slowing in the Los Angeles region, testing positivity continued to increase beyond 10% this week and the county reached over 700 weekly cases per 100,000 residents. The region has now consistently surpassed 10,000 cases daily, and we suspect the ceiling in Los Angeles County is 18,000-20,000 cases daily, which will continue to significantly challenge hospital capacity.
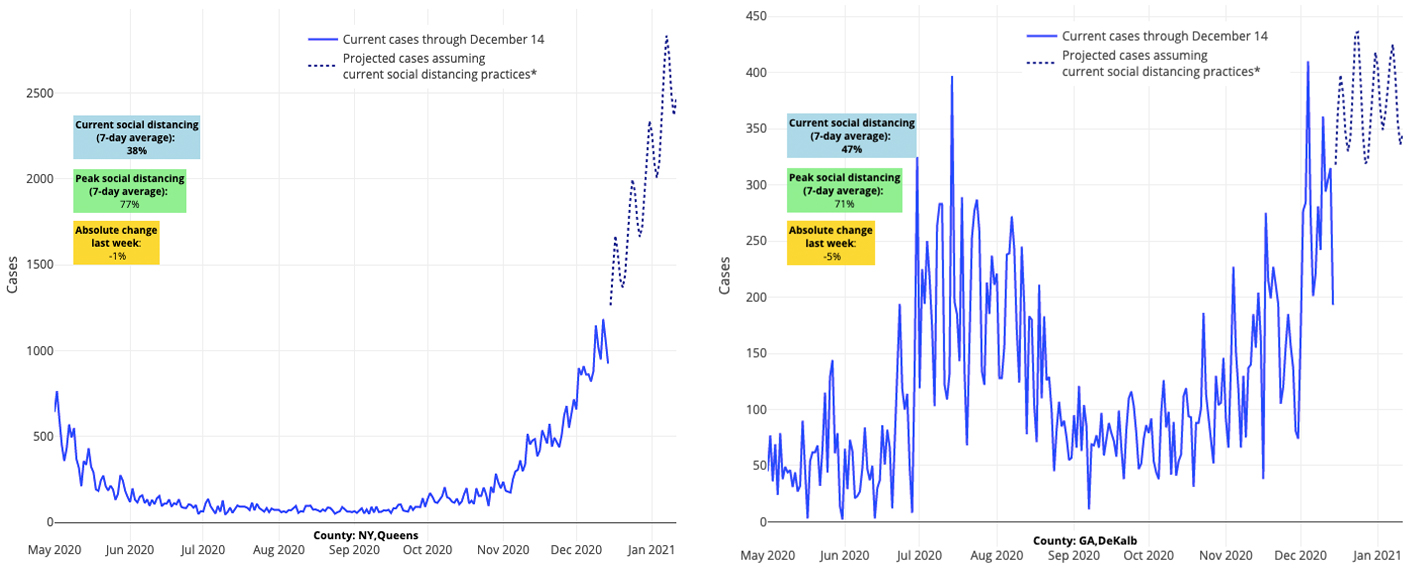
Above are the projections for Queens County in New York (left) and DeKalb County in Georgia (right).
Moving Beyond the Thanksgiving Surge, Challenges Remain
The last great anticipated period for surging viral transmission lies ahead over the next 10 days during the Christmas and New Year’s holidays. Similar to our report last week, we find in our modeling data that while parts of the Midwest are past their peak, we are still nearing peaks in other areas of the county like the Northeast, Southeast, and Sun Belt states, and through California and the Pacific Northwest. We remain particularly concerned about the Southeast, as there remains considerable growth potential in the Carolinas, Georgia, and Tennessee, among other states. New York City gripped our attention in March and April and, according to our projections, will do so again this holiday season.
As with Thanksgiving, we would encourage holiday gatherings to be small this year, despite the tremendous fatigue everyone has for the pandemic. The post-Thanksgiving surge unequivocally demonstrated the risk across generations of gathering and traveling around a holiday. We have watched Los Angeles quickly surge past 10,000 cases daily, and we are witnessing case incidence trends in the Northeast that very much resemble those in the Upper Midwest earlier this fall. Vigilance in our distancing and masking behaviors now can help assure a safer Christmas for many family members.
What the Arrival of the Vaccine Means for the Winter Outlook
With great optimism, vaccines arrived this week, and many health care workers and nursing home residents are already getting their first doses. The immediate impact of this initial vaccination period will be to shore up our health care staff, ensuring that we have the consistent and healthy workforce to shoulder the long lag of rising hospitalizations and hospital capacity strain that we predict will persist well into the winter.
At the peak of the surge in the Upper Midwest this fall, states reported greater than 30% ICU occupancy for COVID patients and local hospital capacity strain was common. We are now seeing similar trends in the Northeast, Southeast and Sun Belt. COVID-19 ICU occupancy is exceeding 40% in Pennsylvania; 35% in Maryland; 30% in New Jersey, Massachusetts and Delaware; and 25% in New York and Connecticut. Further south, Mississippi is moving beyond 40% ICU occupancy of COVID-19 patients and Alabama is surging past 50%. In California, ICU occupancy of COVID-19 patients is greater than 45%, and Arizona is again seeing 40% occupancy, much like in early summer.
COVID-19 patients, shoulder-to-shoulder with non-COVID patients, will test the ability of hospital systems to deliver appropriate access and high-quality care. The vaccination of residents in long-term care facilities will be a huge boost to hospitals and avert continued strain. Within the next month, we should see the rising tide of admissions begin to fall, as the largest group of individuals contributing to increasing hospitalizations become protected.
The Value of Assurance Testing, Even as Vaccines Arrive
While vaccines have started to be distributed, the majority of Americans will still need to recommit to the practices of masking and distancing that will help us manage community transmission in the months ahead. Most loved ones, particularly caregivers and grandparents, will not receive access to vaccinations for months. Schools throughout the country continue to struggle with keeping their doors open, as staffing shortages have been severe, and infections have increased among students and staff alike.
But, while vaccines will not be able to alter the course of most public sectors of life for several months, a growing pipeline of rapid testing is likely on the horizon. Over the fall, many colleges showed the country the path ahead by testing students (often twice) in anticipation of students returning to campuses and then at least weekly thereafter. This form of sentinel surveillance, conducted at universities like Tulane University in New Orleans, the University of Illinois in Champaign and the University of New Hampshire, was largely responsible for reducing infection rates on campuses and assuring safety for the wider communities surrounding colleges.
These experiences join growing evidence on the value of assurance testing. The newly appointed Centers for Disease Control and Prevention (CDC) Director, Dr. Rochelle Walensky authored a report describing the potential impact of weekly testing of college students as an strategy to quickly identify asymptomatic but infectious individuals in order to prevent on-campus outbreaks before they happen. Our team was fortunate to participate in a study with colleagues across Pennsylvania examining the value of such strategies to repopulate college campuses safely, which the CDC cited last month.
The main takeaway from all of this work: as community incidence and infection rates among young adults have risen, frequent testing on college campuses is a preferred strategy for mitigating widespread transmission across the greater campus community.
We not only expect many colleges to adhere to these standards as the new semester arrives, but we would also anticipate the arrival of this type of weekly assurance testing for K-12 school staff and select populations of students. New assurance testing programs are being established in New York City and Texas, and many independent schools have also been moving in this direction since fall. In our own region, we are excited to partner with our local health departments and public school districts as they create their own plans to conduct testing in schools this winter. Our focus now is on assurance testing of school staff and children with special health care and educational needs. For this latter group, masking and/or distancing may be difficult to achieve during the school day; offering frequent testing may greatly improve the safety of these classrooms within the schools.
All told, our country is getting its feet underneath us as Christmas and New Year’s approach, but there is great work yet to be done, and holiday gatherings could potentially further aggravate the tenuous situation that many states now find themselves in. As we near or move past peaks in many areas of the country, we would emphasize that overall risk for infection remains high in most areas and the equilibrium of these peaks remains fragile. That equilibrium is likely highly related to more universal and tighter restrictions around masking and distancing, as well as many families reducing the size of their gatherings between the holidays. It is also possible that the caution many families showed around Thanksgiving seems to have avoided an even more dramatic resurgence in some parts of the country.
We would encourage all to remain vigilant throughout the remainder of this holiday season to avoid another post-holiday surge as we await the promise of vaccine distribution after New Year’s.
