COVID-19 Outlook: Hastened Recovery Continues, Although Some Risk Remains

Following a break from modeling last week, our COVID-Lab team updated our case incidence and hospitalization forecasts today for counties across the country; the models project continued declines in case incidence and hospitalizations over the next four weeks. We project that most regions will see these improvements, although some counties are forecasted to see a leveling off of their declines, warranting close monitoring in the coming weeks.
In addition to reviewing our modeling results, this week’s blog post shares insights from our new study published in Health Affairs, which highlights the benefit masking requirements had earlier in the pandemic, offering some evidence on how these strategies might be used, if needed, during a future public health emergency.
Please note that as long as the current trends continue, we don’t plan to update our projections again until mid-March.
Here is an overview of state-level hospitalization data and projections:
- The national adult hospital census has declined to nearly 65,000 individuals, after having peaked just a few weeks ago at nearly 160,000 patients.
- States with adult hospital censuses that remain greater than 50 patients per 100,000 residents include West Virginia, Kentucky, Alabama and Arkansas. All of these states except Alabama continue to have adult weekly admissions in excess of 40 patients per 100,000 residents.
- The five states with the lowest adult hospital censuses, defined as below 15 patients per 100,000 residents, are all in New England: Vermont, Connecticut, New Hampshire, Massachusetts and Rhode Island.
- National pediatric hospital census has declined 60% from its peak just a few weeks ago.
- More than half of hospitalized children are in the South. States with persistent pediatric hospital census in excess of 5 patients per 100,000 children include Oklahoma, Missouri and Tennessee.
- While our four-week projections show that all states will see declining adult admissions and census, that rate of decline is beginning to slow, particularly in the Northeast and Midwest. The northern parts of the Southeast, like Tennessee, also continue to lag behind other regions in our models with slower declines in hospitalizations continuing for the next few weeks.
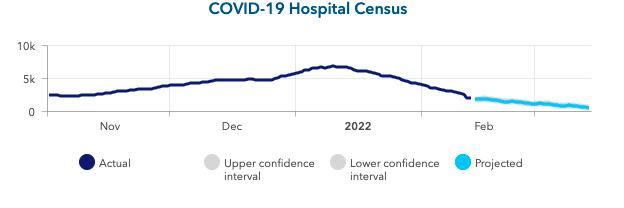
Above is a graph showing COVID-19 hospital census (actual & projected) in Ohio.
Here are county-level updates:
- The national average PCR test positivity rate across the 812 counties included in our model was 15.9% last week, a decline of nearly 50% from just two weeks ago. States with average PCR testing positivity below 5% include Vermont, New York, Illinois, Maryland and Massachusetts.
- The average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) has fallen to 0.56, with 98% of counties now below 1 (up from 85% two weeks ago).
- Average case incidence has fallen to 440 weekly cases per 100,000 residents. One in eight counties are now seeing fewer than 200 weekly cases per 100,000 residents, including Orange County, Calif., Marion County (Indianapolis), Ind., Philadelphia County, Pa., and Essex County (Newark), NJ. Baltimore and Cleveland are reporting fewer than 100 weekly cases per 100,000 residents.
- All of our county-level case incidence projections continue to show declining case incidence over the next four weeks. However, for some counties, particularly in the Northeast and parts of California including Los Angeles, our forecasts suggest that reproduction numbers may hover close to 1 in the coming weeks, which may translate into slower declines in case incidence for these areas.

Above are the projections for Baltimore County in Maryland.

Above are the projections for Los Angeles County in California.
Our Outlook for the Rest of Winter
Our models reveal current and forecasted trends of case incidence and hospitalizations that confirm what the nation has witnessed recently; we are in the midst of a swift recovery that now involves all regions of the country.
While we are excited that counties across the country are experiencing declines in case incidence and hospitalizations, we are mindful that there are some localities where declines in reproduction numbers may slow. Reflecting back on mid-February last year, we note that there was an inflection point that started a brief period of increased case incidence and hospitalizations at the tail end of winter. We hypothesized that gatherings and travel related to the Super Bowl, Valentine’s Day, and Presidents’ Day Weekend led to that late winter increase, and we’re seeing signs that this could occur once again as our forecasts suggest that reproduction numbers will increase over the next four weeks. Fortunately, most counties have low enough reproduction numbers that any increase will not exceed 1. Therefore, case incidence is still projected to decline, but likely at a slower rate than it has recently. As we move past these mid-February holidays, we will closely monitor our forecasts for reproduction numbers. If they are projected to exceed 1 for a county, that could foreshadow a local resurgence in case incidence.
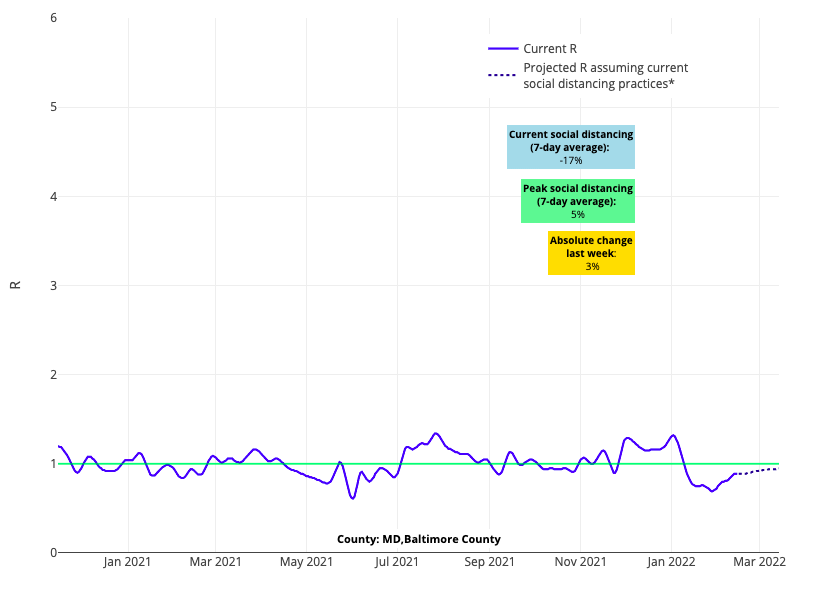
Above is the reproduction number projection for Baltimore County in Maryland.

Above is the reproduction number projection for Los Angeles County in California.
To a certain degree, we should expect declines in case incidence to slow down as numbers fall—that is the natural evolution of an epidemic curve. But we should also not be surprised if some areas stall or even have modest increases in case incidence for a short period of time.
This tail of case incidence in late winter may vary from week to week; for example, some variability may occur as individuals who were extra cautious during the height of this season’s resurgence venture out more as conditions improve. For those who have not yet been exposed to omicron, the risk of transmission remains high enough that some additional infections are possible. This is why public health authorities and the Centers for Disease Control and Prevention (CDC) continue to encourage the use of masks in crowded indoor locations until case incidence improves further. We would encourage schools transitioning to mask-optional policies to inform families of masking recommendations from their local health department and the CDC so that families can make decisions on mitigation strategies during this period based on their own personal circumstances, including health risks to themselves or other family members.
Preparing for future public health emergencies
Health Affairs published yesterday an analysis our team conducted of the impact of county-level masking requirements in the spring and summer of 2020. While the data are from a very different time in the pandemic—when masking in public locations felt especially crucial to protecting each other since we didn’t have vaccines—the results provide valuable insights into the effectiveness of this community-focused measure for future public health emergencies.
While a county-level randomized trial of mask mandates would have been the ideal approach to clearly determine the effectiveness of masking mandates, that study design was not feasible amidst an evolving pandemic. However, our team employed a pragmatic trial design to emulate a randomized trial. Under this design, our study team matched counties with similar geographic and demographic characteristics at the same time point of the pandemic that either implemented a mask mandate or didn’t. For a breakdown of these complex methods, please see Dr. Jing Huang’s blog post.
Overall, this study assessed the experience of nearly 400 counties during March-October 2020. The results revealed that mask mandates were associated with a subsequent reduction in community case incidence. The impact of mask mandates were greatest in large, urban counties and, to some extent, in communities where residents, based on political preferences, may have been more reticent to wear masks in the absence of a mandate. We also found that the greatest reductions in transmission happened six weeks after the start of a mask mandate and began to wane thereafter. Interestingly, we saw little impact in the more rural counties that we studied.
Now, nearly two years later, we are at a different moment in the pandemic and our study’s findings are not applicable to our current situation. We are moving beyond the public health emergency and mask mandates are being lifted in many locations. That said, this retrospective analysis reminds us that there was a time earlier in the pandemic when broad use of masking likely saved many lives, allowing sufficient time for vaccinations to arrive in late 2020. These data can inform the approach to future epidemics or pandemics. When used in a targeted fashion and with clear endpoints, policymakers can implement mask mandates effectively, so long as the limitations of these approaches are recognized, and requirements are removed when they no longer achieve the desired impact.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.
