COVID-19 Outlook: Getting a Head Start on Fall Planning - School Quarantine Protocols

Here are this week’s main findings from the update to our COVID-Lab forecasting model:
- The national average PCR test positivity rate declined to 5.5% (down 0.8% since last week), with a majority of the 821 counties included in our model now reporting testing positivity of less than 5%. The largest declines in testing positivity were in Midwestern, Northeastern, and Mid-Atlantic states; Michigan had the largest absolute decline of any state (down 2.3%).
- Eleven states saw an increase in test positivity rates this week, but only three (Alabama, Washington and Oregon) saw those rates increase by 1% or more.
- The median reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) for the country is down to 0.92, with 60% of all counties in our model below 1. Only 10% of these counties are still experiencing substantial transmission (R>1.25). This is half the number of counties with substantial transmission just two weeks ago.
- Case incidence in most counties we follow is below 100 weekly cases per 100,000 individuals, and only 15% of these counties have a weekly case incidence over 200 cases per 100,000 individuals.
- Nationally, adult hospitalizations continue to fall. Daily COVID-19 admissions have dropped below 7,000, and the number of hospitalized patients is below 40,000. The number of pediatric COVID-19 hospitalizations remained stable, hovering near 1,000.
Specific regional updates:
- Reproduction numbers in all New York City boroughs dropped below 0.8. Our models project substantial declines in case incidence will continue in NYC over the next four weeks.
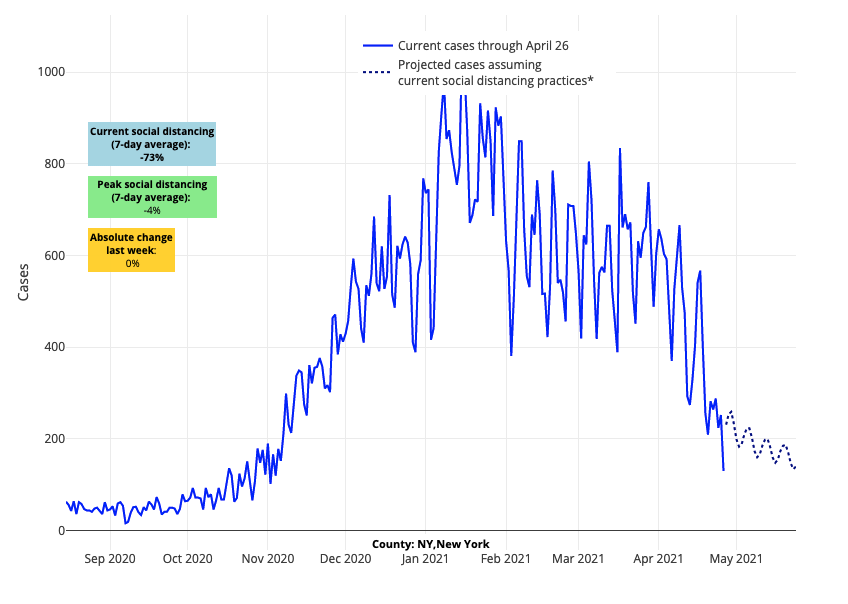
Above are the projections for New York County (Manhattan) in New York.
- Detroit (Wayne County) is now reporting well below 1,000 cases daily, and our models project that this number will drop below 500 in the next couple of weeks. It was only two weeks ago that the county was reporting over 2,000 daily cases. Daily hospital admissions have dropped by 50% and hospital census is falling.
- Declining test positivity and flat hospitalizations in the Carolinas and Florida suggest that these states may also be moving beyond their 2021 spring peak. Other areas of the South, including counties in Tennessee, Georgia, and Alabama, saw increasing transmission and emergency department visits this week, although at much lower rates than over the winter.
- The Phoenix area (Maricopa County) is experiencing rising test positivity and a slight increase in hospitalizations and ICU stays. This will be an area to monitor in the coming weeks.
- Statewide case incidence and hospitalizations, which looked like they might be improving last week, continued increasing in most counties across Colorado. Increasing reproduction numbers and testing positivity have also persisted in many counties. However, case incidence and test positivity improved in its largest city, Denver, where our models project cases will fall over the next four weeks.
- The Pacific Northwest is one area of the country with accelerating test positivity and hospitalization rates. In prior surges, overall impacts in these regions have been small, but case incidence is now well beyond 100 weekly cases per 100,000 individuals and hospitalizations are increasing at a steady rate. However, our models forecast that increases in Seattle will be short lived, reaching its peak this week. The models also project that the Portland metro area, including locations to the south, will sustain increases in case incidence for a bit longer.

Above are the projections for Multnomah County (Portland) in Washington.
Substantial declines in community transmission continue in most areas of the country
For the third week in a row, we see clear evidence that transmission is falling, and will continue to fall, in most regions of the United States. The most significant declines this week were in the New York City metropolitan area, which is a huge relief for a region that has been beset with high transmission for many months. As expected, there remain pockets of increased test positivity rates and case incidence, including the Phoenix area, some counties in the Southeast and parts of the Pacific Northwest. We are hopeful that the increasing trends in these locations will be short lived.
Much of the improvements can be tied to increasing vaccination rates among younger and middle-age adults, which is reducing transmission at social gatherings of similar-aged individuals. Still, we recognize that vaccine coverage varies from community to community. As the nation begins to plateau near a 50% adult vaccination rate, and with growing reports of diminished vaccine eagerness among older youth, it is likely that certain communities will have decreased vaccine coverage. We urge local leaders to continue communicating about the importance of vaccination among their community members. Communities with low rates of vaccination will be more vulnerable to higher transmission of SARS-CoV-2 in the fall. The presence of variant strains, like the B.1.1.7 strain that originated in the United Kingdom, may also enhance fall seasonal transmission, and communities with less vaccine coverage could allow for further emergence of variant strains.
Keeping community transmission rates low through vaccinating adolescents and adults will be particularly important to younger children, as vaccines are not likely to be available to them until winter, or perhaps early 2022.
Preparations for the next school year are beginning – a focus on quarantine procedures
With weeks left in the school year, most schools are taking advantage of proven mitigation strategies alongside declining community transmission to return more students to in-person learning. School leaders are already appropriately discussing plans for the fall, when they hope to launch a more normal school year with many adults and older children vaccinated.
Because COVID-19 transmission is likely to occur during the coming school year, much like other seasonal respiratory viruses, well thought-out safety protocols are essential. The nature of these protocols will depend on community rates of transmission, knowledge of vaccination rates among staff and students beginning the year and, most importantly, the regional guidance that health departments provide. It is too early to predict whether these protocols will require many of the mitigation strategies leveraged this past winter and spring (e.g., mask use, social distancing, quarantine recommendations), but school leaders and public health officials will address these topics upon reviewing data over the summer. Still, any plans will require some flexibility as we progress into the fall and winter seasons when some resurgence is likely to occur.
We will comment more on expectations for summer and early fall community transmission rates, as well as thoughts about masking and distancing in relationship to the 2021-22 academic year, as we review data on transmission and vaccination over the next several weeks. This week, our focus will be on quarantine recommendations for close contacts. Schools should anticipate that quarantine and isolation will remain the backbone of our public health strategy for the foreseeable future, and it will arguably be the biggest challenge for schools next year.
Historically, quarantine has been the most critical public health intervention for disrupting transmission of epidemic respiratory viruses. Therefore, COVID-19 is likely to join whooping cough (pertussis) as a disease that continues to require public health reporting and potential quarantine for individuals who are exposed to an infected individual at school. Such recommendations might change if COVID-19 is found to be less virulent over time, but school communities should anticipate that quarantine restrictions may continue to be a component of public health guidelines next year, particularly in the winter.
Schools are not without options as they prepare for quarantine protocols next year. The simplest approach for schools that do not have access to testing will be a traditional 10-day quarantine for children who are exposed at school to another child or adult with COVID-19, but who remain asymptomatic. But, for those who have access to rapid testing, quarantines in most locations can be abbreviated to one week with a negative test for an individual who remains asymptomatic. While there will be much debate on the footprint of testing in schools next year, the use of testing for shortening quarantine restrictions is likely to be a strong consideration for schools investing, even at this late date, in testing capabilities for next year. New federal funding for school-based testing, at the very least, should equip many schools with staffing and access to tests.
As a third approach, our team increasingly believes we have reached a moment when school-based testing might offer an alternative for exposed children who stay asymptomatic to remain in school if they participate in thrice-weekly testing. While the rate of infection among those exposed to COVID-19 at school is not inconsequential—in our region, more than 700 children have been tested to shorten the length of quarantine through Project: ACE-IT, and 4.5% of the elementary-age children and 2.8% of the high school youth were positive (overall rate: 3.3%)—it is still of a magnitude that “test-to-stay” approaches might be appropriate for the 95% or more of students without COVID-19 who would miss extended days of school for quarantine. Testing children immediately after exposure and every 2-3 days the following week could conceivably decant risk to schools.
To proceed forward, health departments would likely require evidence that schools could appreciably accomplish a minimum of testing all students out of quarantine before they might approve the transition to a “test-to-stay” program. Our team recognizes that such an approach would be an unconventional application of quarantine restrictions, but we also appreciate the compromise it provides for keeping children in school during an uncertain time. Offering choices to schools around quarantine protocols is also superior to modified quarantine where children remain in school during the quarantine period without testing. The rates we are observing among exposed children, alongside continued concerns about emerging variant strains, would not support that approach at this time.
As schools commence their planning for next year, most things will return to normal, but some challenges will remain. We are in the process as a country of accommodating to a virus that is unlikely to be completely eradicated. This last year our daily lives were upended by this once-in-a-lifetime pandemic; restrictions, necessary though they were, dramatically impacted our way of life. As difficult as it was to accommodate these restrictions, it can be even more difficult to undo them. We are beginning that process carefully and looking forward to assisting school leaders in the journey ahead.
