Achieving Birth Equity for Minority Women Means Addressing Their Stress
Editors Note: PolicyLab’s communications team is interested in learning more about our blog readers and your thoughts on our content. We invite you to take this 5-minute survey to help us ensure our posts continue to be helpful and relevant to our readers. The survey will be open until May 1, 2019.
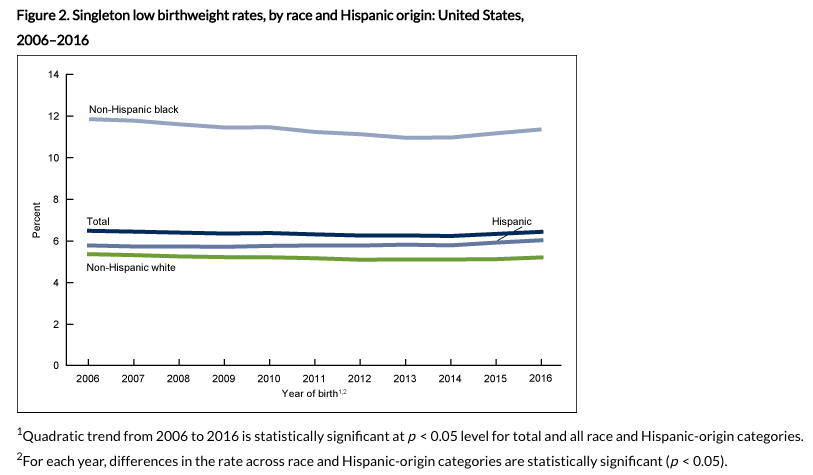
Walk into any neonatal intensive care unit (NICU) and you will see many striking things. Babies that could fit in the palm of your hand. Babies with more tubes than you could imagine might fit on those tiny bodies. But one of the most striking things you will always find is how many African-American babies there are. It is not an illusion; racial and ethnic disparities in infant health outcomes have been well-documented and persistent for decades. African-American women in this country still deliver 50% more preterm infants than non-Hispanic white mothers. In addition, the infant mortality rate among African-American infants is over twice that of non-Hispanic white infants.
Health disparities have been defined in many ways, but the definition I appreciate the most is that they are “systematic, plausibly avoidable health differences adversely affecting socially disadvantaged groups” from Paula Braveman, MD, MPH, director of the Center on Social Disparities in Health at the University of California, San Francisco. Vexingly, research focused on risk factors associated with birth outcome disparities have failed to fully explain what my colleagues and I see in the NICU every day. Even after accounting for the socio-economic risk factors—such as the quality of their health insurance and how much education they have received—and behavioral factors related to tobacco use or engagement with the health care system, African-American women in this country continue to experience disproportionately higher rates of morbidity and mortality in their infants and themselves.
Concerningly, as we begin to more closely examine the perinatal outcomes of other racial/ethnic minority groups, we are beginning to see that health outcomes may not be as “good” across the board for other minority women—such as Hispanics—as we previously believed.
So, what do we know? For some time now, we have widely accepted that both acute and chronic stress can have harmful impacts on health. Anyone who has ever been in a stressful situation is familiar with the repercussions; you can’t sleep, you can’t focus, you change how you interact with friends, family and coworkers in ways that can damage those relationships. Unfortunately, many women live in a constant state of stress and anxiety, and researchers are increasingly considering a mother’s stress during pregnancy the link between the reality of factors associated with disadvantage (e.g., living in a poor neighborhood, poor access to quality food, discrimination) and racial disparities in birth outcomes. Researchers have also linked the experience of stress to a disruption in many normal physiologic processes, the premature aging of the immune system and heightened risk for development of illness. Furthermore, studies of African-American women suggest that they tend to experience heightened stress related to discrimination, socio-economic hardship, living in poor neighborhoods and acculturation.
Given the link between disparities in adverse birth outcomes and these heightened levels of stress related to systematic discrimination and institutionalized social disadvantage, one glaring question that researchers must ask is, “How?” How exactly is the experience of stress in African-American women implicated in a baby being born early or dying early? How are known causes of preterm birth triggered by stress-related changes to a mother’s physical health? To answer these questions, we must turn to the literature on how stress affects the human body and understand one very important term, “allostatic load.”
Allostatic load refers to the physical burden placed on the body when someone is consistently exposed to physical and emotional stress. Researchers have actually discovered many important biological markers that indicate allostatic load is present in a person. The literature exploring allostatic load, particularly as it relates to adverse birth outcomes and their associated disparities, is promising but ripe for study as there are many gaps, particularly when it comes to pregnancy. As more and more markers are considered indicators of allostatic load, we still don’t know which ones are the best indicators of adverse birth outcomes. Furthermore, there is early evidence that these markers may differ among people of different income, education and racial backgrounds. Thus, to better understand how allostatic load works in pregnancy, researchers must ensure that diverse participants are included in studies that examine the relationship between stress, pregnancy and infant health.
But stepping for a moment into a universe in which we know how to best measure and document allostatic load in diverse research study populations, we still have to address the fundamental issue of heightened stress experienced by disadvantaged individuals and communities in our society. Ultimately, the questions become policy related as the focus shifts from a biologic “how” into an interventional “how” and its sister question “when.” How are we going to implement broad-scale screening of chronic physiology-altering stress at the level of the population? When should screening occur if we are to impact reproductive outcomes? Some would argue that screening during pregnancy is far too late if the intent is to reverse the impact of allostatic load. Similarly, when in a woman’s life should we implement interventions aimed at stress management and resilience-building in order for them to have the most impact on her reproductive health?
It is crucial that the impact of stress on a woman’s lifetime risk of poor reproductive outcomes is beginning to be recognized. However, it is time we recognize that maternal stress is amplified by systematic racism and disadvantage and that this has significant public health ramifications for our health care system and society. This is especially true if we consider that allostatic load may even be altering a woman’s biology in such a way that she passes on the risk of poor birth outcomes to future generations. Therefore, our research must seek evidence-based strategies to intervene on the pathologic consequences of stress on a woman’s own body while we also seek to dismantle the larger socio-structural determinants that caused her stress in the first place. Maybe then can the striking things I see in the NICU every day become only the extent to which medicine is able to help the littlest of patients and not the overwhelming face of a deep disparity.